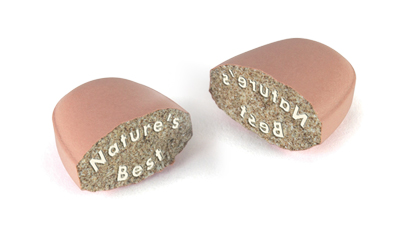
Trust your gut, Trust our Science.
Save up to £4 on ProBiome live bacteria.
Scientifically researched bacterial strains.
Delayed-release technology.
Strains reach the gut alive to thrive

July Offers
Explore a wide range of popular products at discounted prices
Big savings on best sellers
Multi-buy bargains
Discounts on supplements, pet health, and aromatherapy oils

Omegas
Boost heart health, enhance brain function, support flexibility and promote overall wellness with our premium fish oil supplements!
Outstanding purity
Responsible sourcing
Trending Products

Probiome Everyday

Probiome Sensitive

Probiome for Travel

Lecithin Granules

Anxiety
Discover supplements and expert tips to support anxiety management effectively.

Bone Health
Explore our comprehensive range of bone health products and specialised formulas.

Brain Health
Support cognitive health with our exceptional range of brain health supplements.

Tiredness & Fatigue
Support your energy levels with our exceptional range of expertly crafted supplements.

Gut Health
Nurture your gut health with our specialised range of supplements for comprehensive support.

Heart Health
Support heart health with our specialised range of supplements for cardiovascular wellness.

Immunity
Support immune health with these essential nutrients and comprehensive range of multivitamins.

Memory
Discover brain-friendly nutrients such as herbs and vitamins to support cognitive function.
Men's Health
Explore our tailored range of supplements for men of all ages.

Women's Health
Discover our specialised supplements for women of all ages, tailored to their unique needs.

Omega 3s
Premium-grade UK-made fish oil supplements. Friend of the Sea® certified. Freshness guaranteed, responsibly sourced.

Colladeen®
Anthocyanidins, natural plant pigments, widely researched for their role in skin health.
Multivitamins
Discover expert multi-vitamins with age and gender-based formulas for optimal nutrition.

Glucosamine
Quality Glucosamine supplements with complementary nutrients for an active lifestyle.

Turmeric
Exceptional quality turmeric supplements crafted from premium-grade raw materials sourced from reputable suppliers.

Herbs & Spices
Support well-being with our range of herbal heroes, including Ginkgo, Palmitoylethanolamide, lutein, and more.

CoQ10 & Ubiquinol
Shop our range of all-natural CoQ10 (ubiquinone) and body-ready ubiquinol supplements.
Digestion
A supplement range designed by nutrition experts to support the digestive system.
Buy With Confidence At Nature's Best

About Nature's Best
Founded in 1981 and now one of the UK’s best loved nutritional supplement suppliers. Leaders in nutrition science with over 250 products in our range, amazing service and FREE expert nutrition advice.

Nutrition Buzz
Access an extensive range of health and wellness articles, offering expert advice into the world of vitamins, minerals and supplements. Discover practical tips and knowledge to empower you in your pursuit to wellbeing.

Free Expert Advice
We have a team of friendly Expert Nutrition Advisors that provide FREE individual help and advice, so that customers can make the right choice about their health and supplement regime.

Catalogue Requests
Request a copy of our catalogue and discover our extensive range of products. Thoughtfully designed to assist you in navigating through more than 250 vitamins, minerals, and supplements. Additionally, explore our assortment of aromatherapy essential oils and nourishing health foods. A must-read resource for leisurely browsing and exploring our exciting collection.
Shop Our Top Products
120 capsules, 1-a-day, 4 month supply
(621 reviews)High strength. Excellent level for anyone on statins as they deplete CoQ10. Useful level for heart and gum health. In a vegetable oil base
£29.95£25.95
120 tablets, 3 daily, 1 month supply
(1437 reviews)No. 1 best seller. Glucosamine and chondroitin plus rosehips, ginger, quercetin and MSM for active lifestyles. 3- a - day vegan tablet
£15.95£13.95
180 tablets, 1-a-day, 6 month supply
(550 reviews)A one-a-day formula delivering the full 375mg of magnesium. Essential magnesium that's taste- free, easy to swallow and gentle on the tummy.
£13.95
60 tablets, 1-a-day, 2 month supply
(700 reviews)One of the UK's strongest Lutein supplements for eye health. Pure Lutein with Zinc and extracts of Bilberry and Blackberry. Unique formula, UK-Made.
£20.95£17.81
90 tablets, 1 to 3-a-day, up to 3 month supply
(444 reviews)High strength tablets with 800mg of free plant sterols per tablet and high levels of beta-sitosterols. Contributes to the maintenance of normal cholesterol levels.
£15.95
100 tablets, 1-a-day, 3 + month supply
(196 reviews)Often chosen by vegetarians. Essential for red blood cell formation. High strength, from just 5.53p/day. Small, easy to swallow tablets. One-a-day.
£4.95
60 tablets, 2-a-day, 1 month supply
(385 reviews)Formulated to provide nutrients known to support the body's defences against sun damage to skin. Same strength as Colladeen® Original plus lutein and green tea.
From £20.95
60 tablets, 1-a-day, 2 month supply,
(2023 reviews)A perfect partner to glucosamine. Also used as a digestive. One of the UK's strongest and purest one-a-day formulas.
£18.95£15.95
120 capsules, 1-a-day, 4 month supply
(621 reviews)High strength. Excellent level for anyone on statins as they deplete CoQ10. Useful level for heart and gum health. In a vegetable oil base
£29.95£25.95
120 tablets, 3 daily, 1 month supply
(1437 reviews)No. 1 best seller. Glucosamine and chondroitin plus rosehips, ginger, quercetin and MSM for active lifestyles. 3- a - day vegan tablet
£15.95£13.95
180 tablets, 1-a-day, 6 month supply
(550 reviews)A one-a-day formula delivering the full 375mg of magnesium. Essential magnesium that's taste- free, easy to swallow and gentle on the tummy.
£13.95
60 tablets, 1-a-day, 2 month supply
(700 reviews)One of the UK's strongest Lutein supplements for eye health. Pure Lutein with Zinc and extracts of Bilberry and Blackberry. Unique formula, UK-Made.
£20.95£17.81
90 tablets, 1 to 3-a-day, up to 3 month supply
(444 reviews)High strength tablets with 800mg of free plant sterols per tablet and high levels of beta-sitosterols. Contributes to the maintenance of normal cholesterol levels.
£15.95
100 tablets, 1-a-day, 3 + month supply
(196 reviews)Often chosen by vegetarians. Essential for red blood cell formation. High strength, from just 5.53p/day. Small, easy to swallow tablets. One-a-day.
£4.95
60 tablets, 2-a-day, 1 month supply
(385 reviews)Formulated to provide nutrients known to support the body's defences against sun damage to skin. Same strength as Colladeen® Original plus lutein and green tea.
From £20.95
60 tablets, 1-a-day, 2 month supply,
(2023 reviews)A perfect partner to glucosamine. Also used as a digestive. One of the UK's strongest and purest one-a-day formulas.
£18.95£15.95

Focus of the month:
Gut Health
Gut Health
Explore articles on how to support your digestive health, emphasising nutrition, lifestyle changes and helpful supplements.
Save Even More With Our Affiliates

Emergency services discount

Armed Forces and Veterans

Men & Women 55+

Student discount

Student, apprentice or aged 16-26