Healthy vision is something many of us take for granted, especially when we’re young. But as we get older we may start to notice our eyesight isn’t as good as it used to be. And if our vision continues to worsen it can have a serious impact on our wellbeing by affecting our social lives, our ability to stay mobile and by increasing our risk of having accidents and serious injuries.
Indeed, age is the most significant risk factor for the development of eye disease. According to the RNIB, there are 1.2 million people living with sight loss in the UK who are aged 75 years and overi. So what exactly happens to your eyes as you age? And what practical steps can you take to support your eyes in your 40s, 50s, 60s and beyond?
Eyes and ageing
It’s normal for your eyes and vision to change during the course of your lifetime. As you get older, you may experience one or more of the following:
-
You need more light to see well
-
You struggle to see things close up, such as newspaper print
-
Bright lights cause more glare at night
-
You see colours less vividly
-
Your eyes feel more dry and irritated
The good news is all of these things are a normal part of getting older.
At what age do eyes start to deteriorate?
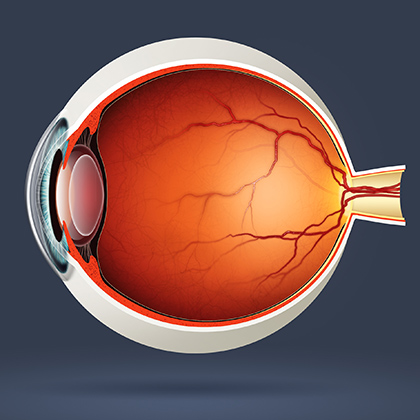
One of the first things to be affected by age in the eye is the lens. This starts to become thicker and less flexible when you reach your 40s, as a result of muscles in the eye that surround the lens called ciliary muscles becoming tighterii. When this happens, the lens cannot change shape as easily as it used to, which means it cannot focus effectively on near objectsii.

This condition is called presbyopia – or age-related long-sight (hypermetropia) – and it affects nearly everyone as they get olderiii. At first you may notice you’re having difficulties reading the small print, but eventually, you may not be able to focus on close objects at all. Find out more on the impact of presbyopia here.
Do eye muscles weaken with age?
Your pupils also become smaller because the muscles that make them expand and contract don’t work as they used toiv. This also means they don’t react as quickly as they used to when suddenly exposed to bright light, and they contract more slowly in the dark.
Having smaller pupils means you need more bright light to see properly (when reading, for example) while looking at bright lights at night can cause more glare than you saw beforeiv. The fact that your pupils start reacting to light and dark more slowly can mean you’ll be dazzled momentarily when you go outside in bright conditions, and your eyes may take longer than usual to get used to the dark when you switch off your lights at night.
The muscles in your eyelids that make them open and close also get weaker as you get older. This can sometimes cause a condition called ectropion that affects some older people, where the lower eyelid turns outwards from the eye.
Getting older also means your body produces fewer tears, leading to dryness and irritation. This is particularly common in women after the menopause. Ageing gradually reduces your peripheral vision too, and the cells in part of your eye called the retina that helps you to see colours become less sensitive, making colours less bright and with reduced contrastiv.
Another thing you may notice as you get on in years is the appearance of floaters, tiny spots or specks that drift around your field of vision. These can be irritating, but they’re usually normal and harmless, caused by the gel-like substance inside the eye called the vitreous pulling away from the retinav. Floaters are also common in younger people who’ve had eye surgery.
What’s the most common eye condition related to ageing?
Presbyopia is considered the most common physiological age-related change affecting the eyesvi. Other common eye conditions related to ageing include age-related macular degeneration, glaucoma, cataracts and diabetic retinopathy:
Macular degeneration
Also commonly called age-related macular degeneration (or AMD for short), this is an eye disease that affects part of the retina at the back of the eye called the macula. The macula is a tiny area that allows you to see fine detail and colours. But if it becomes damaged, it can cause central vision loss. Your peripheral vision, meanwhile, remains unaffected.
What’s your risk?
The estimated number of people with AMD in the UK is currently 4.8 per cent of those aged 65 and older and 12.2 per cent of those aged 80 and older, with around 70,000 new diagnoses each yearvii. But while age is the most significant risk factor, some other things can increase your risk of AMD, including:
-
Smoking
-
Gender (women have a higher risk than men)
-
High blood pressure
-
A family history of AMD
-
Obesity
AMD symptoms
Central blurring in your vision, visual distortions, sensitivity to light and seeing straight lines as wavy or fuzzy.
How is it treated?
There are two types of AMD – dry AMD and wet AMD. Dry AMD currently cannot be treated, but if you have wet AMD you may need regular eye injections to prevent any further deterioration in your vision.
Glaucoma
A group of eye diseases where the optic nerve that connects the eye to the brain becomes damaged, glaucoma can cause peripheral vision loss. It’s usually caused by increased pressure inside the eye caused by a build-up of fluid in the front part of the eye.
What’s your risk?
You can get glaucoma at any age, but it’s most common in people in their 70s and 80sviii. Besides age, things that can increase your risk of glaucoma include:
-
A family history of glaucoma
-
High blood pressure
-
Diabetes
-
Short-sightedness and long-sightedness
Glaucoma symptoms
Glaucoma is often painless and can have no symptoms, but some people experience signs such as blurred vision and seeing rainbow-coloured halos around bright lights. If glaucoma develops suddenly it can cause extreme eye pain, nausea, vomiting, headache, eye redness and tenderness around the eye.
How is it treated?
Glaucoma can often be treated with eye drops that help lower the pressure in the eye. Laser treatment to reduce fluid in the eye or surgery to boost the drainage of fluid may also be recommended in some cases.
Cataracts
A cataract is when the lens in your eye – which is normally clear – becomes cloudy, causing blurred and unclear vision (and, if untreated, blindness). Cataracts are the most common cause of vision loss worldwide, and here in the UK around one in three people aged 65 or older is thought to be affected by themix,x.
What’s your risk?
Again, age is the most common risk factor for cataracts. But other things may increase your risk too, such as:
-
Smoking
-
A family history of cataracts
-
Diabetes
-
Eye injury/trauma
-
Drinking too much alcohol
-
Taking some medicines long term, such as steroids
Cataract symptoms
Cataracts usually develop so gradually you may not notice anything for a few years. However, if you find your eyesight is becoming blurred or misty, when you find it increasingly difficult to see well in low light conditions when colours look faded or you see more glare with bright lights, ask your optometrist (optician) for advice.
How is it treated?
Cataracts just get worse over time if you don’t do anything about them. The only effective treatment is surgery to remove the cloudy lens and replace it with a new, artificial one.
Diabetic retinopathy
If you have diabetes, you may experience a complication called diabetic retinopathy. This is when the blood vessels that supply the retina become damaged, causing bleeding and swelling of the retinal tissue. As a result, your vision can become cloudy, and if left untreated diabetic retinopathy can lead to blindness.
What’s your risk?
According to the NHS, anyone with type 1 or type 2 diabetes is potentially at risk of developing diabetic retinopathyxi. However, your risk is greater if you’ve had diabetes for a long time or any of the following:
-
Persistent high blood glucose
-
High blood pressure
-
High cholesterol
Your risk is also greater if you’re pregnant or you’re of South Asian, Black African or Caribbean backgroundi.
Diabetic retinopathy symptoms
If you have diabetes the signs of diabetic retinopathy should be picked up early during regular diabetic eye screening. However, if you’ve noticed your vision getting gradually worse if you have blurred or patchy vision, eye pain, eye redness, sudden vision loss or floaters, see your GP or diabetes care team as soon as possible.
How is it treated?
Laser treatment, eye injections and eye surgery are used to treat an advanced stage of diabetic retinopathy. You can stop the condition deteriorating by managing your diabetes and keeping your blood sugar levels under control, as well as managing your blood pressure and cholesterol, keeping them within healthy levels.
Six tips for healthy eyes
Seeing your optometrist for regular eye check-ups is essential for keeping your vision healthy, as they can usually pick up the signs of age-related eye problems long before you experience any related symptoms. Eye tests are free on the NHS, and are usually recommended every two years – but if you’re 40 or older, you may need them more often.
There are also other things you can do to keep your eyes as healthy as possible, especially as you get older, including the following:
1. Eat healthily
A healthy balanced diet can help maintain healthy eyes and you manage your weight, which in turn reduces your risk of developing conditions such as high blood pressure, heart disease, stroke and type 2 diabetes – all of which can lead to vision problems. The NHS also suggests cutting down on salt, fat and sugar to protect against diabetic retinopathyxii. According to the RNIB, evidence also suggests that having a diet rich in fruit and vegetables may help keep your eyes healthyi.
2. Stay active
Exercising regularly will also help keep your weight in check. Aim to do at least 150 minutes of moderate-intensity exercise such as walking or cycling each week.
3. Drink alcohol in moderation
If you drink heavily, your risk of developing early AMD may be higher than normal, says the NHSxiv. Government recommendations for moderate drinking – which aims to keep the health risks from alcohol at a low level – include drinking no more than 14 units a week on a regular basis (for men and women), spreading your drinking over three or more days if you regularly drink as much as 14 units a week, and trying to have several drink-free days each week.
4. Protect your eyes from the sun
You may be used to protecting your skin from the sun’s damaging UV rays, but do you also protect your eyes? Looking at the sun directly is very dangerous, and can cause irreversible damage to your eyesight. And according to the NHS, there’s evidence to suggest sunlight exposure is a risk factor for cataractsxiv. Wearing sunglasses can help – look for a good-quality dark pair with a built-in UV filter (check they carry the CE mark or British Standard BS EN ISO 12312-1).
5. Give up smoking
According to the NHS, smokers are more likely to develop AMD and cataracts than non-smokers. The RNIB also claims smoking doubles your chances of losing your sight, and can also make diabetes-related sight problems – such as diabetic retinopathy – worsexiii. If you need help with quitting, try stop smoking methods such as nicotine patches, gum and lozenges.
6. Take natural supplements
There are a number of nutritional supplements available that are designed to maintain and improve eye health, including certain types of antioxidants, omega-3 fatty acids found in fish oils and ginkgo biloba.
For further information on natural supplements for eye health as well as loads more about eye conditions and top tips to help keep your eyes healthy, take a look at the rest of our Vision Health Hub articles.
References:
-
Eye health and sight loss stats and facts Available online: https://www.rnib.org.uk/sites/default/files/Eye%20health%20and%20sight%20loss%20stats%20and%20facts.pdf
-
Mayo Clinic. (2017). Presbyopia: Symptoms & Causes, Diagnosis & Treatment. Available online: hhttps://www.mayoclinic.org/diseases-conditions/presbyopia/symptoms-causes/syc-20363328 [Accessed 28 Jan. 2019].
-
All About Vision. (2018). Presbyopia. Available online: https://www.allaboutvision.com/conditions/presbyopia.htm [Accessed 28 Jan. 2019].
-
MSD Manual. (2016). Effects of Aging on the Eyes. Available online: https://www.msdmanuals.com/en-gb/home/eye-disorders/biology-of-the-eyes/effects-of-aging-on-the-eyes [Accessed 28 Jan. 2019].
-
All About Vision. (2017). How Your Vision Changes As You Age. Available online: https://www.allaboutvision.com/over60/vision-changes.htm [Accessed 28 Jan. 2019].
-
Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2040246
-
Lowth, M., Tidy, C. Patient. (2016). Age-Related Macular Degeneration. Available online: https://patient.info/doctor/age-related-macular-degeneration-pro
-
NHS. (2018). Glaucoma. Available online: https://www.nhs.uk/conditions/glaucoma [Accessed 28 Jan. 2019].
-
World Health Organization. (2018). Blindness and Vision Impairment Prevention. Available online: https://www.who.int/blindness/causes/priority/en/index1.html [Accessed 28 Jan. 2019].
-
GP Online. (2011). Treatment Of Cataracts. Available online: https://www.gponline.com/treatment-cataracts/ophthalmology/article/1078013 [Accessed 28 Jan. 2019].
-
NHS. (2018). Diabetic Retinopathy. Available online: https://www.nhs.uk/conditions/diabetic-retinopathy [Accessed 28 Jan. 2019].
-
NHS. (2018). Prevention: Diabetic Retinopathy. Available online: https://www.nhs.uk/conditions/diabetic-retinopathy/prevention [Accessed 28 Jan. 2019].
-
RNIB. (2018). Nutrition & the Eye. Available online: https://www.rnib.org.uk/eye-health/looking-after-your-eyes/nutrition-and-eye [Accessed 28 Jan. 2019].
-
NHS. (2018). Healthy Body: Look After Your Eyes. Available online: https://www.nhs.uk/live-well/healthy-body/look-after-your-eyes [Accessed 28 Jan. 2019].
Related Posts?
Disclaimer: The information presented by Nature's Best is for informational purposes only. It is based on scientific studies (human, animal, or in vitro), clinical experience, or traditional usage as cited in each article. The results reported may not necessarily occur in all individuals. Self-treatment is not recommended for life-threatening conditions that require medical treatment under a doctor's care. For many of the conditions discussed, treatment with prescription or over the counter medication is also available. Consult your doctor, practitioner, and/or pharmacist for any health problem and before using any supplements or before making any changes in prescribed medications.

Christine
Christine Morgan has been a freelance health and wellbeing journalist for almost 20 years, having written for numerous publications including the Daily Mirror, S Magazine, Top Sante, Healthy, Woman & Home, Zest, Allergy, Healthy Times and Pregnancy & Birth; she has also edited several titles such as Women’ Health, Shine’s Real Health & Beauty and All About Health.
View More