It goes without saying that as you get older you’ll develop one or two wrinkles and a few more grey hairs than you’d like. But ageing also brings about other changes in our bodies – including in our hearts, bones, joints, brain and even our eyes. All these changes can lead to age-related problems, with one of the most common affecting vision being age-related macular degeneration (AMD).
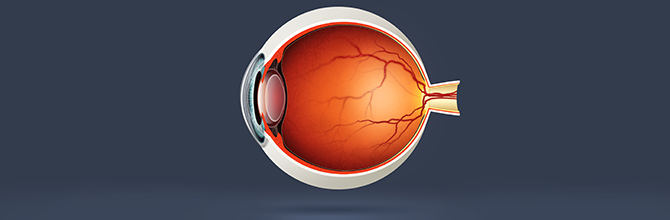
According to the Royal College of Opthalmology, AMD is the name for changes caused by ageing that happen in the central area of the eye’s retina – called the macula – in people aged 55 and olderi. It can cause severe visual impairment, so if you’ve recently been diagnosed with AMD it can be very worrying. This guide aims to provide information about your condition and give you the guidance and support you may need.
What is AMD?
AMD affects the middle part of your vision, making it distorted or blurry. Affecting one or both eyes it can progress and, over time, you can develop a blank patch in the centre of your vision.
Your peripheral vision – or side vision – isn’t affected. However, losing your central vision can have a significant impact on your seeing, causing difficulties with things like reading, writing, driving, watching TV and recognising faces. But because you still have peripheral vision AMD doesn’t cause complete blindness, and you should still be able to see enough to remain independent and be aware of objects and people.

AMD also doesn’t cause pain. The first thing you may notice is that part of your vision is distorted – when reading, for instance, the words in the centre of the page may look blurred, or straight lines may look wavy or crooked. You may also find you need brighter light than usual for reading, or that colours seem more faded.
How quickly your symptoms develop will depend on which type of AMD you have:
Dry AMD
The most common type of AMD develops slowly and it may be years before your vision becomes seriously affected. It happens when parts of the macula become thinner with age, which means they cannot work properly, and when deposits called drusen build up behind the macula. There is no treatment for dry AMD, but some people may find vision aids such as magnifying glasses, large print, gadgets with big buttons and very bright lighting can be helpful. According to the American Optometric Association, some experts also believe there’s a link between nutrition and the progression of dry AMD, which means that making dietary changes and taking supplements may help slow down AMD-related vision lossii (see below for more details).
Wet AMD
While this is far less common than dry AMD, it can develop very quickly – often in just days or weeks – and can cause severe vision loss. Also sometimes called neovascular or exudative AMD, it happens when cells in the macula stop working correctly, which triggers the growth of new blood vessels. These blood vessels leak blood and fluid, which damages cells in the macula and eventually causes scarring. Treatment is available for wet AMD that stops new blood vessels from growing and damaging the macula. However, you need to be treated quickly, before too much damage has been done.
Some people may be more susceptible to AMD than others. Age is the biggest risk factor, but you may also be more likely to develop AMD if you…
-
Smoke
-
Have high blood pressure
-
Have AMD in your family
-
Have been exposed to high levels of sunlight
-
Are obese
What can you do?
If you’re in your 50s or older and haven’t been diagnosed with AMD, it’s important to go for regular eye tests to have your eyes checked for the early symptoms of AMD as well as other eye conditions such as glaucoma.
Other things you could do to protect your vision include giving up smoking, wearing sunglasses in sunny conditions and maintaining a healthy weight.
Meanwhile, if you have diagnosed AMD, you may benefit from eating certain foods and taking certain nutritional supplements:
Lutein and zeaxanthin
These are natural plant pigments called carotenoids, both of which are found in high concentrations in the macular (studies suggest people with AMD have lower-than-normal amounts of macular pigmentiii).
Indeed, a study involving people with AMD suggests taking a lutein supplement may help improve vision as well as boost levels of macular pigmentiv. Earlier research shows people with higher amounts of lutein and zeaxanthin in their diets may have a reduced risk of AMDv. Find out how to get more lutein and zeaxanthin in your diet by reading What Foods Contain Lutein and Zeaxanthin: Eating for Eye Health.
Fish oils
It’s believed that fish oil may support eye health in general, with the American Optometric Association suggesting that low levels of the omega-3 fatty acids found in oily fish – eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) – are associated with AMDvi.
There is evidence that omega-3 fatty acids may help protect against AMD: one study found eating oily fish at least once a week may halve your odds for developing wet AMD7; meanwhile, a landmark study called the Age-Related Eye Disease Study (AREDS) found those eating the most omega-3 fatty acids may be 30 per cent less likely to develop AMD than people eating the leastviii.
Find out more about the benefits of omega-3 fatty acids for vision in our article Exploring the Eye Health Benefits of Omega 3.
There’s lots more information on the link between diet, nutritional supplements and AMD – as well as other eye conditions – in Healthy Eyes: Dietary Considerations to Improve Your Vision and Supplementation for Eye Health: What Does Science Say?
Managing your wellbeing
If you have AMD it can take a toll on your emotions, especially if you’ve just been diagnosed. According to the UK’s Macular Society, many people with AMD experience feelings of isolation, shock, fear, anger and disbelief, followed by low self-esteem or depressionix.
The society offers a helpline manned by specialist staff who can offer support and provide information and advice about all aspects of vision loss – call 0300 3030 111 to chat to someone in confidence.
Meanwhile, there are a few more things you could do to boost your self-esteem and your mental wellbeing in general:
Learn as much as you can
Knowledge is power, as they say, so gather as much information as you can about your condition. Speak to your doctor or ophthalmologist, and ask your local social services what aids may be available to make everyday life easier and safer.
Join a group
Talking to other people who have experienced what you’re going through can help you feel you’re not alone. The RNIB has a community for people affected by sight loss called RNIB Connect – call 0303 123 9999 or visit the RNIB website. The Macular Society also has a network of almost 300 local groups, one of which may be in your area (call 0300 3030 111 or email help@macularsociety.org).
Stay connected
Keeping in touch with your friends and family – even when you feel tempted to stay away – can help you feel more independent and in control, as well as reduce your risk for depression and other health conditions.
Take a look around the rest of our Vision Health Hub for lots more information on eye conditions as well as lots of advice about keeping your eyesight healthy.
References:
-
Age-Related Macular Degeneration: Guidelines for Management. The Royal College of Opthalmologists. Available online: https://www.rcophth.ac.uk/wp-content/uploads/2014/12/2013-SCI-318-RCOphth-AMD-Guidelines-Sept-2013-FINAL-2.pdf
-
Available online: https://www.aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/macular-degeneration
-
Landrum, J.T., Bone, R.A., Kilburn, M.D. The macular pigment: a possible role in protection from age-related macular degeneration. Adv Pharmacol. (1997) ;38:537-556. Available online: https://www.sciencedirect.com/science/article/pii/S10543589086099
-
Richer, S., Stiles, W., Statkute, L., et al. Double-masked, placebo-controlled, randomized trial of lutein and antioxidant supplementation in the intervention of atrophic age-related macular degeneration: the Veterans LAST study (Lutein Antioxidant Supplementation Trial). Optometry. 2004 75:216-30. Available online: https://www.ncbi.nlm.nih.gov/pubmed/15117055
-
Seddon, J.M., et al. Dietary carotenoids, vitamins A, C, and E, and advanced age-related macular degeneration. Eye Disease Case-Control Study Group. JAMA. 1994 Nov 9 ;272(18):1413-20. Available online: https://www.ncbi.nlm.nih.gov/pubmed/7933422
-
Available online: https://www.aoa.org/patients-and-public/caring-for-your-vision/diet-and-nutrition/essential-fatty-acids
-
Augood, C., et al. Oily fish consumption, dietary docosahexaenoic acid and eicosapentaenoic acid intakes, and associations with neovascular age-related macular degeneration. Am J Clin Nutr. 2008 Aug. 88(2):398-406. Available online: https://www.ncbi.nlm.nih.gov/pubmed/18689376
-
AREDS Research Group, ω–3 Long-chain polyunsaturated fatty acid intake and 12-y incidence of neovascular age-related macular degeneration and central geographic atrophy: AREDS report 30, a prospective cohort study from the Age-Related Eye Disease Study. The American Journal of Clinical Nutrition, Volume 90, Issue 6. 1 December 2009. Pages 1601–1607. Available online: https://academic.oup.com/ajcn/article/90/6/1601/4598106
-
Emotional impact of sight loss Macular Society. Available online: https://www.macularsociety.org/sites/default/files/resource/Macular%20Society%20Emotional%20Impact%20of%20Sight%20Loss.pdf
Related Posts?
Disclaimer: The information presented by Nature's Best is for informational purposes only. It is based on scientific studies (human, animal, or in vitro), clinical experience, or traditional usage as cited in each article. The results reported may not necessarily occur in all individuals. Self-treatment is not recommended for life-threatening conditions that require medical treatment under a doctor's care. For many of the conditions discussed, treatment with prescription or over the counter medication is also available. Consult your doctor, practitioner, and/or pharmacist for any health problem and before using any supplements or before making any changes in prescribed medications.

Christine
Christine Morgan has been a freelance health and wellbeing journalist for almost 20 years, having written for numerous publications including the Daily Mirror, S Magazine, Top Sante, Healthy, Woman & Home, Zest, Allergy, Healthy Times and Pregnancy & Birth; she has also edited several titles such as Women’ Health, Shine’s Real Health & Beauty and All About Health.
View More



