Every woman’s cycle is different. Although a typical menstrual cycle is 28 days, with a period lasting around 5 days, this is just an average (1). Regular cycles that range from 21 to 40 are also perfectly normal.
Those with PCOS, however, often experience irregular or absent menstrual cycles due to hormone imbalances, which affect ovulation. And this may lead to challenges with conception and family planning.
Fortunately, there are many simple ways to support hormone regulation and bring some balance to your monthly cycle.
What are irregular periods?
Your menstrual cycle serves as a unique window into how your body’s working, and when something’s not as it should be.
Healthcare providers describe irregular periods as those that fall outside ‘regular’ ranges. If you have an irregular cycle, your periods may happen infrequently, frequently, or unpredictably.

Menstrual irregularities might mean that it can be harder to fall pregnant because it often means you don’t ovulate (release an egg) regularly.
There are many causes of irregular periods. But certain medical conditions, like PCOS, can be a risk factor.
Light or infrequent periods (oligomenorrhea)
Oligomenorrhea occurs when your periods are more than 35 days apart. Women with light, infrequent periods tend to have four to nine periods a year.
Oligomenorrhea often happens when girls recently started menstruating. Some young women don’t have a regular cycle for several years after their first period, which is considered normal and not usually a cause for concern.
If your cycle varies by a few days from one month to the next, again, it’s not generally considered irregular. Some women have a period every three weeks, others every five – either way, it’s nothing out of the ordinary unless you have periods that are fewer than three weeks or more than five weeks apart.
However, hormone imbalances – such as those experienced by women with PCOS – are often behind missed and delayed periods.
Frequent periods (polymenorrhea)
Having a period of fewer than 21 days apart is known as polymenorrhea. If you have polymenorrhea, your periods may also be irregular and/or unpredictable.
Polymenorrhea may affect your fertility since it means you ovulate sooner in your cycle than you should ordinarily.
Heavy periods (menorrhagia)
During a normal period, a woman may lose around 30ml of blood. But if you have a heavy flow, you may lose more. Losing more than 60ml of blood is classed as ‘menorrhagia’. Heavy periods can also be painful and may last more than seven days.
To determine if you have heavy periods, consider how many tampons and/or pads you use daily. If you need an excessive amount of sanitary protection or bleed through clothes or bedding, you may have menorrhagia.
Though heavy periods aren’t anything too serious to worry about, they can affect you emotionally and physically – not to mention disrupt your everyday life.
Abnormally light periods (hypomenorrhea)
Unlike menorrhagia, hypomenorrhea describes a very light flow and short periods. Taking the contraceptive pill or using another hormone-based method of contraception is known to cause abnormally light periods. This isn’t known to cause fertility problems any more than having a normal cycle.
Absent periods (amenorrhoea)
Amenorrhoea is the absence of menstruation, often defined as missing one or more periods.
There are two types of amenorrhoea:
-
Primary amenorrhoea: this occurs when a woman hasn’t started having periods by the age of 16
-
Secondary amenorrhoea: this occurs when a woman previously had regular periods but they stopped for at least three months
Painful periods (dysmenorrhoea)
Dysmenorrhoea refers to painful abdominal cramps during menstruation. You may also feel discomfort in your lower back and the tops of your thighs.
Primary dysmenorrhoea is caused by the uterus contracting and is often accompanied by heavy periods.
Secondary dysmenorrhea is caused by another condition, like endometriosis or uterine fibroids.
Causes of irregular periods
It’s normal to have some variability in the length of your cycle (2). But if your cycle has been unpredictable for a while, there may be another explanation.
-
The first few years after starting your period (menarche) (3)
-
Pregnancy
-
After pregnancy (4)
-
Perimenopause (the years before your menstrual cycle ends, which can happen around the age of 45). Once in perimenopause, cycle length can vary between 14 and 50 days, though some women report little changes (5).
-
Starting or stopping hormonal contraception, such as the pill or IUD (6)
-
Jet lag, shift work, or long-distance travel (7)
-
Extreme weight loss or weight gain, increased stress, or excessive exercise (8)
-
Certain medical conditions, like a thyroid disorder or PCOS (9).
How does PCOS cause irregular periods?
Every month, your ovaries release a follicle to be fertilized. However, since PCOS causes hormonal imbalances, leading to higher levels of androgens, like testosterone and the luteinizing hormone, the tiny follicle doesn’t mature or get released (10).
Instead of being released, the rebellious follicle (often called a ‘cyst’) remains in the ovaries. High levels of circulating testosterone can disrupt your menstrual cycle and prevent ovulation (11).
Without regular ovulation and the normal biological events that lead to it, your uterus doesn’t have the momentum required to shed its lining. And this can cause oligomenorrhea or infrequent periods.
PCOS period pain
PCOS is known to affect the flow and regularity of your periods. But there’s little research to suggest it may be to blame for severe period pain. Though enlarged ovaries with cysts could be behind menstrual discomfort, it’s more likely there’s another condition at play.
If you already have PCOS and experience debilitating period pain, there’s a chance you may have endometriosis, which can make menstruation incredibly painful. It’s unusual to have PCOS and endometriosis, but it’s not impossible, so always have a chat with your GP if you’re concerned. Find out more about endometriosis and the difference between the two conditions here.
How to treat irregular periods and period pain
If you have PCOS and experience irregular periods or painful periods, don’t worry. There are several treatments and management tools available to support your menstrual health.
Medical interventions
It’s always wise to speak to a healthcare professional if you have consistent rather than occasional period problems, such as irregular periods, heavy or painful periods, or periods that last more than seven days.
While the contraceptive pill isn’t a magic bullet, health professionals often prescribe it to women with PCOS as a first line of defence – alongside lifestyle changes – to improve menstrual cycle irregularities.
Although birth control triggers an ‘artificial’ period, this bleed keeps many other important physiological functions working. A regular menstrual bleed will support bone health, for instance.
It’s also worth mentioning that some medications may interfere with your menstrual cycle, so you may wish to discuss this with your GP if you take any regular medication.
Lifestyle changes
Making simple changes to your lifestyle can also support menstrual regularity and improve overall hormonal health with PCOS.
Maintain a healthy weight
Carrying excess weight can affect menstrual regularity due to the impact fat cells can have on insulin and hormones.
Though PCOS can make weight loss harder, losing even a small amount of weight can reduce PCOS symptoms and support menstrual health (12). You can learn more about PCOS weight gain and tips for PCOS weight loss here.
Extreme weight loss can also lead to irregular periods, so it’s important to maintain a healthy, moderate weight.
Exercise
In combination with a balanced diet, regular exercise can support weight loss and weight maintenance, which, in turn, may help regulate your menstrual cycle.
Research suggests physical activity may also help dysmenorrhoea, making it a great addition if you have PCOS period pain (13).
Moving little and often is one of the best ways to increase your overall activity. You may wish to invest in a standing desk, park further away from the entrance at work or any destination, have walking meetings, or exercise during your lunch break.
Reduce stress
High levels of stress can have a knock-on effect on your menstrual cycle. Stress releases cortisol and adrenaline, hormones that make it harder for insulin to work properly, which may lead to and worsen menstrual irregularity.
Having a bank of stress-fighting hacks could make a big difference to your menstrual health. Journaling, meditation, laughter, and quality sleep can all help buffer against stress. Just find what works for you.
Mind-body practices, like yoga and tai chi, are another great way to reduce stress, improve menstrual regularity, and support PCOS symptoms more generally (14).
Yoga is also associated with less menstrual pain and fewer emotional symptoms associated with PMS (15).
Supplement support
In addition to medical interventions and simple lifestyle changes, you may wish to add the following supplements to your diet for more targeted support.
Myo-inositol
Myo-inositol might be the most important supplement if you experience irregular periods with PCOS.
Many women with PCOS are insulin resistant, meaning their bodies can make insulin but can’t use it properly.
Insulin resistance often causes the body to produce more androgens, ‘male’ hormones like testosterone, and alter the balance of luteinizing (LH) and follicle-stimulating hormone (FSH). These hormonal imbalances can disrupt ovulatory patterns (16).
Research suggests myo-inositol can decrease insulin resistance, which may help restore hormones to a ratio needed for ovulation (17).
Though relatively small-scale, one study reported that myo-inositol supported ovulation and improved fertility in women with PCOS (18).
The recommended dose of myo-inositol for women with PCOS is 2 grams in the morning and 2 grams in the evening. For convenience, choose powdered myo-inositol and mix it with water or juice.
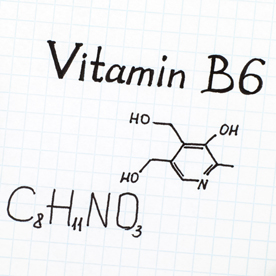
B vitamins
The B vitamins are involved in a number of important biological processes. Specifically, vitamin B6, folate, and vitamin B12 are known to support hormone balance in PCOS. These nutrients help break down homocysteine, which is commonly elevated in women with PCOS (19). High homocysteine levels are associated with menstrual irregularities and reduced fertility (20).
Though you can find B vitamins in many foods, including leafy vegetables, beans, and organ meats, taking a quality B vitamin complex may help buffer your natural reserves.
Magnesium
Magnesium plays a critical role in over 300 biochemical processes in the body. Research suggests those with PCOS are 19 times more likely to experience a magnesium deficiency than the general population (21).
Low magnesium may exacerbate insulin resistance, which can affect hormone balance. Evidence suggests magnesium may improve insulin sensitivity and PMS symptoms (22).
You can find magnesium in whole grains, dark leafy vegetables, beans, and legumes. But it might be an idea to add a magnesium supplement to your diet to support your intake.
Vitamin D3
Although vitamin D3 is a vitamin, it’s regarded as more of a hormone. This is because it influences many systems in the body, including the immune system, endocrine system, cardiovascular system, and other metabolic pathways (23).
Lower levels of vitamin D3 have been associated with ovulatory and menstrual irregularities, so increasing your intake may support hormone balance (24).
Aside from getting 10-15 minutes of unprotected, direct sunlight every day and eating more food naturally rich in vitamin D3, such as oily fish, egg yolks, cheese, and liver, you may also want to take a high-strength supplement.
Find out more about PCOS
Irregular periods can be one of the most challenging and frustrating symptoms to navigate for women with PCOS, especially because they can affect fertility. But we hope it brings you some comfort knowing there are simple measures you can take to restore balance to your menstrual cycle.
If you want to learn more about PCOS periods – or anything else related to PCOS – take a look at our dedicated health hub. Alternatively, please get in touch with our team of expert Nutrition Advisors, who are on hand to provide free, confidential advice.
References:
-
NHS choices. (2023) Available online: https://www.nhs.uk/conditions/periods/fertility-in-the-menstrual-cycle/
-
Fehring RJ, Schneider M, Raviele K., Variability in the Phases of the Menstrual Cycle. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2006;35(3):376–84.
-
Jackson E, Glasier A., Return of Ovulation and Menses in Postpartum Nonlactating Women: A Systematic Review. Obstetrics & Gynecology. 2011;117(3):657–62.
-
Hale GE, Robertson DM, Burger HG., The perimenopausal woman: Endocrinology and management. The Journal of Steroid Biochemistry and Molecular Biology. 142, 121–31.
-
Davis AR, Kroll R, Soltes B, Zhang N, Grubb GS, Constantine GD., Occurrence of menses or pregnancy after cessation of a continuous oral contraceptive. Fertility and Sterility. 89, 5, 1059–1063.
-
Mahoney MM., Shift work, jet lag, and female reproduction. International Journal of Endocrinology.
Fernandez RC, Marino JL, Varcoe TJ, Davis S, Moran LJ, Rumbold AR, et al., Fixed or Rotating Night Shift Work Undertaken by Women: Implications for Fertility and Miscarriage. Seminars in Reproductive Medicine. 34, 2, 74–82. -
Huhmann K., Menses Requires Energy: A Review of How Disordered Eating, Excessive Exercise, and High Stress Lead to Menstrual Irregularities. Clinical Therapeutics. 42, 3, 401–7.
-
American College of Obstetricians and Gynecologists Practice Committee Bulletins—Gynecology. (2018) ACOG Practice Bulletin No. 194: Polycystic Ovary Syndrome. Obstet Gynecol. 131(6):e157–71.
Jacobson MH, Howards PP, Darrow LA, Meadows JW, Kesner JS, Spencer JB, et al. (2018) Thyroid hormones and menstrual cycle function in a longitudinal cohort of premenopausal women. Paediatr Perinat Epidemiol. 32(3):225–34. -
Rosenfield RL, Ehrmann DA. (2016) The Pathogenesis of Polycystic Ovary Syndrome (PCOS): The Hypothesis of PCOS as Functional Ovarian Hyperandrogenism Revisited. Endocrine Reviews. 37(5):467–520.
-
Rosenfield RL. (2016) The Pathogenesis of Polycystic Ovary Syndrome. Endocrine Reviews. 37(5):467–520.
-
Marzouk TM, Sayed Ahmed WA. (2015) Effect of Dietary Weight Loss on Menstrual Regularity in Obese Young Adult Women with Polycystic Ovary Syndrome. J Pediatr Adolesc Gynecol. 28(6):457-461.
-
Cronk, Nikole PhD; Zweig, Alex MD; Deane, Kristen MD. (2021) Is exercise an effective treatment for dysmenorrhea? Evidence-Based Practice 24(7): 2-33.
-
Rani M, Singh U, Agrawal GG, Natu SM, Kala S, Ghildiyal A, Srivastava N. (2013) Impact of Yoga Nidra on menstrual abnormalities in females of reproductive age. J Altern Complement Med. 19(12): 925-929.
-
McGovern, C.E. and Cheung, C. (2018) Yoga and quality of life in women with primary dysmenorrhea: A systematic review. Journal of Midwifery & Women’s Health. 63(4): 470-482.
-
Diamanti-Kandarakis E, Dunaif A. (2012) Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocrine Reviews. 33(6): 981-1030.
-
Asimakopoulos G, Pergialiotis V, Anastasiou E, et al. (2020) Effect of dietary myo-inositol supplementation on the insulin resistance and the prevention of gestational diabetes mellitus: study protocol for a randomized controlled trial. Trials. 21, 633.
-
Papaleo E, Unfer V, Baillargeon JP, De Santis L, Fusi F, Brigante C, Marelli G, Cino I, Redaelli A, Ferrari A. (2007) Myo-inositol in patients with polycystic ovary syndrome: a novel method for ovulation induction. Gynecol Endocrinol. 23 (12): 700-703.
-
Günalan E, Yaba A, Y?lmaz B. (2018) The effect of nutrient supplementation in the management of polycystic ovary syndrome-associated metabolic dysfunctions: A critical review. J Turk Ger Gynecol Assoc. 19 (4): 220-232.
-
Ebisch IM, Peters WH, Thomas CM, Wetzels AM, Peer PG, Steegers-Theunissen RP. (2006) Homocysteine, glutathione and related thiols affect fertility parameters in the (sub)fertile couple. Hum Reprod. 21 (7): 1725-33.
-
Sharifi F, Mazloomi S, Hajihosseini R, Mazloomzadeh S. (2012) Serum magnesium concentrations in polycystic ovary syndrome and its association with insulin resistance. Gynecol Endocrinol. 28 (1): 7-11.
-
Hamilton KP, et al. (2019) Insulin Resistance and Serum Magnesium Concentrations among Women with Polycystic Ovary Syndrome. Current Developments in Nutrition. 3, 11, nzz108.
-
Ellison DL, Moran HR. (2021) Vitamin D: Vitamin or Hormone? Nurs Clin North Am. 56(1):47-57.
-
Rashidi B, Haghollahi F, Shariat M, Zayerii F. (2009) The effects of calcium-vitamin D and metformin on polycystic ovary syndrome: a pilot study. Taiwan J Obstet Gynecol. 48(2):142-7.
Related Posts?
Disclaimer: The information presented by Nature's Best is for informational purposes only. It is based on scientific studies (human, animal, or in vitro), clinical experience, or traditional usage as cited in each article. The results reported may not necessarily occur in all individuals. Self-treatment is not recommended for life-threatening conditions that require medical treatment under a doctor's care. For many of the conditions discussed, treatment with prescription or over the counter medication is also available. Consult your doctor, practitioner, and/or pharmacist for any health problem and before using any supplements or before making any changes in prescribed medications.

Olivia
Olivia Salter has always been an avid health nut. After graduating from the University of Bristol, she began working for a nutritional consultancy where she discovered her passion for all things wellness-related. There, she executed much of the company’s content marketing strategy and found her niche in health writing, publishing articles in Women’s Health, Mind Body Green, Thrive and Psychologies.
View More