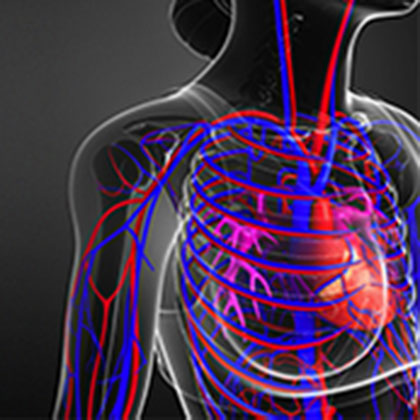
If a vein becomes inflamed because the blood inside it develops into a clot, the condition is called superficial thrombophlebitis. Some people often confuse this with deep vein thrombosis (DVT). But the two conditions are quite different, and one – DVT – is much more serious than the other.
DVT is a blood clot in a deep vein, but in superficial thrombophlebitis the clot develops in a vein near the surface of the skin (superficial veins), often a varicose vein and most commonly a vein in a leg.
Unlike DVT superficial thrombophlebitis isn’t usually serious, though rarely it can develop into a DVT if the clot travels along the superficial vein and into a deeper vein where the superficial and deep veins join together. It is, however, very common, particularly in people aged 60 or older (though anyone of any age – even children – can be affected) (i).
Women are thought to be more at risk of superficial thrombophlebitis than men (i), and one study suggests the condition could also be more common during warmer weather (ii).
What are the symptoms?
If you have superficial thrombophlebitis you may experience swelling, redness and tenderness on an area of skin that covers the affected part of a superficial vein, along with painful, hard or knobbly lumps under the skin. The area of skin affected may also feel itchy or irritated.
These symptoms – which often develop gradually – are usually found on the lower part of the leg, though sometimes a surface vein on an arm, a breast or on the penis can be affected. And while it can be painful, superficial thrombophlebitis shouldn’t stop you carrying on with your daily routine, though sometimes it can be accompanied by a high temperature.
The inflammation usually settles after a few weeks though any lump could take up to four months to disappear, during which time it may still feel quite tender. You may also be left with a darker patch of skin afterwards.
Thankfully the clots associated with superficial thrombophlebitis aren’t usually anything to worry about, since they are usually small, and because other veins bypass the affected vein your blood flow isn’t blocked. However, if the affected vein is a varicose vein, there’s a chance the symptoms will keep coming back.
Other types of phlebitis
Phlebitis means inflammation of a vein, and superficial thrombophlebitis is just one of the different types:
-
Superficial phlebitis is when a vein at the surface of your skin is affected, but there is no clot.
-
Deep phlebitis is when part of a deeper, larger vein – usually in a leg but sometimes also in an arm – becomes inflamed, but with no clot.
-
Deep vein thrombophlebitis is inflammation of a deep vein accompanied by a clot. The most serious type of phlebitis, this can lead to a potentially life-threatening condition called pulmonary embolism. However, it isn’t the same as a DVT, which is when a clot forms in a deep vein but without any inflammation of the blood vessel lining.
What causes superficial thrombophlebitis
Sometimes there’s no obvious reason why superficial thrombophlebitis develops. However, a local trauma or injury to the vein can trigger it, while having an intravenous injection or being given intravenous medicines in hospital (IV drip), for instance. This type of injury can also be common in people who inject recreational drugs.
Some other things can also make you more likely to develop superficial thrombophlebitis, including:
-
Having varicose veins
-
Being very overweight
-
Being a smoker
-
Taking hormone-based medicines such as the contraceptive pill or hormone replacement therapy (HRT)
-
Being pregnant
-
Having a medical condition that can cause blood clots (thrombophilia, for example)
-
Having cancer
-
Having had a blood clot previously or another problem with the vein (a DVT, for instance)
-
Being inactive for a long time, such as during a long journey or if you’re bedridden during an illness or following major surgery
Are there any complications?
Most cases of superficial thrombophlebitis resolve fairly quickly, and most people affected make a full recovery. Complications are uncommon, but they can include the following:
Infection
The affected vein can become infected in some situations, such as if you have a drip inserted for a long time, if you have a weakened immune system or if you inject recreational drugs. The infection can make the pain worse as well as cause a feeling of general unwellness. It can, however, be treated with antibiotics – though a severe infection may need hospital treatment.
DVT
If the clot travels into a deep vein, it can develop into a DVT. This can happen when the clot is near a point where the superficial and deep veins meet, such as in the crease behind the knee or in the upper thigh or groin. Superficial thrombophlebitis is also more likely to progress to a DVT if you’ve had a DVT before, if you’re immobile or if it develops in a normal, rather than a varicose, vein.
Symptoms to look out for include suddenly worsening pain, swelling of the entire leg, and spreading of the inflammation around the back of your knee or calf or up to the inner thigh or groin. If you develop breathing problems or chest pain, this could be a sign that a clot from a DVT has broken off and has travelled to your lung. If you notice any of these symptoms, see a doctor immediately.
Treatments for superficial thrombophlebitis
Even though superficial thrombophlebitis isn’t usually harmful, you should see your GP for a diagnosis, as they may want to make sure you’re not at risk of developing a DVT and check whether or not you have any problems with blood clotting. If your symptoms are mild you won’t usually need any treatment and you should be able to manage any pain and swelling yourself at home. The NHS has the following advice (iii):
-
Raise your leg to help reduce swelling – try to elevate your foot higher than your hip when you’re at rest and also while you sleep.
-
Wear compression stockings to reduce swelling if your GP thinks they may be suitable.
-
Stay as active as possible to keep your blood circulation working.
-
Ease pain by placing a cold flannel over the affected area (other sources suggest a hot flannel may be effective (iv) ).
-
If you need more pain relief, you can also take anti-inflammatory painkillers such as aspirin or ibuprofen or use an anti-inflammatory cream or gel if the affected area of skin is small. Check with your doctor or pharmacist before using anti-inflammatory medicines, as they aren’t suitable for everyone (if you can’t take anti-inflammatories, paracetamol may be a good alternative).
-
Hirudoid cream, which contains an ingredient called heparinoid, may help relieve pain and inflammation, and is available over the counter at pharmacies.
Your doctor may recommend daily injections of a drug called fondaparinux (or Aristra) if necessary to reduce your risk of DVT or pulmonary embolism. You may also be referred to a hospital or a special DVT clinic if your risk of developing a DVT is high.
How can you help yourself?
Your GP will advise you to stay active and keep up with your usual routine, but also try to build more activity into your life by taking the stairs rather than the lift or an escalator and try replacing short car journeys by walking or cycling. Try to avoid sitting or standing for long periods of time – for instance, if you sit all day at work, set a timer to go off every hour to remind you to get up and walk around.
While sitting watching TV you can also keep your legs moving by raising and lowering your heels, then raising and lowering your toes, as well as tightening and releasing your leg muscles.
Your diet could also make a difference, as some foods are thought to help support blood vessel health and keep blood flowing effectively. According to the US-based HeartMD Institute, the best foods for improving your circulation include the following:
Oily fish
Fish such as salmon, mackerel, sardines, trout, fresh tuna and pilchards are rich in omega-3 essential fatty acids that may help reduce inflammation and keep blood flowing more easily.
Nuts
As well as healthy fats and protein, nuts contain magnesium – which helps arteries relax – and the amino acid L-arginine, which is used to produce nitric oxide, a compound that also helps arteries dilate.
Beetroot
Beets also help your body produce nitric oxide as they’re rich in nitrate.
Fruit and vegetables
The vitamin C in fruit and vegetables such as berries, citrus fruits, broccoli, peppers, kiwifruit and tomatoes may also be beneficial for circulatory health, since vitamin C is needed for the body’s production of collagen, an important component of capillary walls.
Garlic
A substance in garlic called allicin is thought to help arteries dilate. As allicin is degraded quickly by heat, try to eat your garlic as raw as possible (add it to cooking at the last possible moment).
Dark chocolate
One or two small pieces of dark chocolate a day could actually be good for you, thanks to the cocoa flavonoids dark chocolate contains. Flavonoids are antioxidants, which may be useful for preventing inflammation.
Meanwhile, the HeartMD Institute also recommends avoiding foods such as added sugars, hydrogenated fats and salt if you want to keep your circulatory system in good shape.
More nutritional support
Adding circulation-boosting foods to your diet may be helpful if you have superficial thrombophlebitis. But there are a few nutritional supplements that may offer additional support too, including the following:
Turmeric
This widely-used culinary spice has many alleged medicinal properties, thanks arguably to its active ingredient curcumin. Experts believe it may benefit a range of inflammatory conditions (v). Commonly used to colour food and add flavour to curry dishes, turmeric is also available as a nutritional supplement.
High-strength fish oils
The omega-3 fatty acids found in oily fish are also thought to act as an anti-inflammatory (vi), with studies suggesting they’re as effective as anti-inflammatory painkillers such as ibuprofen (vii). Oil from cold-water fish is thought to be the richest natural source of omega-3 fats, but you can also get the same omega-3 fats found in oily fish in algae and algae-based supplements, which is good news for vegetarians and vegans.
Anthocyanidins
These compounds – as well as their derivatives anthocyanins – give plant foods such as blueberries, aubergines, cherries and blackberries their deep, rich colours, and are thought to support blood vessels, with one review suggesting that eating them in foods or as extracts significantly improves vascular health (viii).
Gingko biloba
In traditional Chinese medicine, tea made from ginkgo seeds has been used for various health problems. These days, however, ginkgo extracts are made from the tree’s leaves, not the seeds. Many nutritional practitioners recommend ginkgo for boosting blood flow in circulatory disorders. For example, studies suggest it may be modestly effective for circulation problems in the legs caused by a condition called intermittent claudication (ix). Another study suggests ginkgo promotes blood flow improvements in people with heart disease by increasing nitric oxide levels in the body (x).
Superficial thrombophlebitis may not be serious but it can have an impact on your daily routine – this guide may help to ease some of the symptoms. For even more information on a range of other health conditions, feel free to visit our health library.
References:
-
Available online: https://patient.info/doctor/superficial-thrombophlebitis-pro
-
Kakkos. S.K., et al. Seasonal variation in the incidence of superficial venous thrombophlebitis. Thromb Res. (2010 Aug). 126(2):98-102. Available online: https://www.ncbi.nlm.nih.gov/pubmed/20553952
-
Available online: https://www.nhs.uk/conditions/phlebitis
-
Available online: https://patient.info/heart-health/varicose-veins-leaflet/superficial-thrombophlebitis
-
Aggarwal. B.B., Harikumar. K.B. Potential therapeutic effects of curcumin, the anti-inflammatory agent, against neurodegenerative, cardiovascular, pulmonary, metabolic, autoimmune and neoplastic diseases. Int J Biochem Cell Biol. (2009 Jan). 41(1):40-59. Available online: https://www.ncbi.nlm.nih.gov/pubmed/18662800
-
Chin KY. The spice for joint inflammation: anti-inflammatory role of curcumin in treating osteoarthritis. Drug Des Devel Ther. 2016 Sep 20;10:3029-3042.Available online: https://www.ncbi.nlm.nih.gov/pubmed/27703331
-
Lelli D. et al, Curcumin use in pulmonary diseases: State of the art and future perspectives. Pharmacol Res. 2017 Jan /span>;115:133-148.Available online: https://www.ncbi.nlm.nih.gov/pubmed/27888157
-
Calder PC. Omega-3 fatty acids and inflammatory processes: from molecules to man. Biochem Soc Trans. 2017 Oct 15 ;45(5):1105-1115.Available online: https://www.ncbi.nlm.nih.gov/pubmed/28900017
-
Maroon. J.C., Bost. J.W. Omega-3 fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain. Surg Neurol. (2006 Apr). 65(4):326-31. Available online: https://www.ncbi.nlm.nih.gov/pubmed/16531187
-
Fairlie-Jones. L., et al. The Effect of Anthocyanin-Rich Foods or Extracts on Vascular Function in Adults: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Nutrients. (2017 Aug). 9(8): 908.
-
Pittler. M.H., Ernst. E. Ginkgo biloba extract for the treatment of intermittent claudication: a meta-analysis of randomized trials. Am J Med. (2000). 108:276-281. Available online: hhttps://www.ncbi.nlm.nih.gov/pubmed/11014719
-
Wu. Y.Z., et al. Ginkgo biloba extract improves coronary artery circulation in patients with coronary artery disease: contribution of plasma nitric oxide and endothelin-1. Phytother Res. (2008 Jun). 22(6):734-9.. Available online: https://www.ncbi.nlm.nih.gov/pubmed/18446847
Related Posts
Disclaimer: The information presented by Nature's Best is for informational purposes only. It is based on scientific studies (human, animal, or in vitro), clinical experience, or traditional usage as cited in each article. The results reported may not necessarily occur in all individuals. Self-treatment is not recommended for life-threatening conditions that require medical treatment under a doctor's care. For many of the conditions discussed, treatment with prescription or over the counter medication is also available. Consult your doctor, practitioner, and/or pharmacist for any health problem and before using any supplements or before making any changes in prescribed medications.

Christine
Christine Morgan has been a freelance health and wellbeing journalist for almost 20 years, having written for numerous publications including the Daily Mirror, S Magazine, Top Sante, Healthy, Woman & Home, Zest, Allergy, Healthy Times and Pregnancy & Birth; she has also edited several titles such as Women’ Health, Shine’s Real Health & Beauty and All About Health.
View More