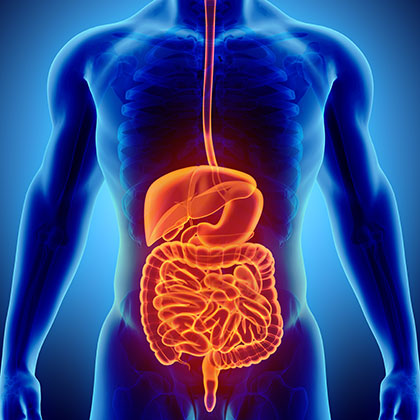
The colon - or large intestine - is an important part of your digestive system. Not only does it help your body to extract some of the nutrients and water from the food you’ve eaten, but it’s also involved in eliminating undigested waste products from your body, pushing them down into the end of the large bowel (the rectum) and out through the anus.
When small bulges or pockets form in the lining of the colon, they are called diverticula (why this happens in some people, nobody really knows).
According to the NHS, the majority of people with diverticula have no symptoms (i). This is known as diverticulosis. Having diverticula is very common. Around half of all people have them by the time they reach the age of 50, with nearly 70 percent of all people having diverticula by the time they are 80 years old (ii).
But when diverticula are accompanied by symptoms such as intermittent lower abdominal pain and bloating – which happens in 25 percent of people with diverticula (ii) – the condition is called diverticular disease.
Diverticula can also become inflamed and infected when bacteria become trapped inside them. This causes more severe symptoms such as constant cramping pain that usually starts below your belly button and most commonly moves to the lower left-hand side of your abdomen, a high temperature, chills, nausea and diarrhoea. When this happens, the condition is known as diverticulitis.
A small number of people with diverticular disease or diverticulitis can develop complications - though these are fairly uncommon - including the following:
-
Abscesses that develop outside the colon are the most common complication of diverticulitis. Some are easily treated with antibiotics, while others may need to be drained under local anaesthetic.
-
Peritonitis, caused by an infection that leads to inflammation of the peritoneum (the layer of tissue that lines the inside of the abdomen). This can happen if infected diverticula split. It can be life-threatening, but it’s rare.
-
Colon blockage: a total or partial blockage can be caused by scar tissue that forms around inflamed diverticula. A total blockage can lead to peritonitis, while a partial blockage can cause a lot of pain. Again, this is very rare.
-
Bleeding from the rectum can also happen in cases of diverticular disease or diverticulitis. Most people affected do not experience pain, and the bleeding usually stops quickly by itself. In a few cases, however, bleeding can be severe, and hospital treatment - including a blood transfusion - is often necessary.
If you think you may have the symptoms of diverticular disease or diverticulitis, see your GP as soon as you can, as it’s important to rule out other conditions that have similar symptoms, including bowel cancer, irritable bowel syndrome (IBS) and pancreatitis.
Diverticular disease and diverticulitis: are you at risk?
Developing diverticula becomes more common as you get older, with being aged 50 or older one of the main risk factors (ii).
However, only around one in four people with diverticula goes on to develop diverticular disease, with 75 per cent of people with diverticular disease having at least one episode of diverticulitis (ii).
Common risk factors
Besides age there are certain things that may increase your risk of developing diverticular disease and diverticulitis, including the following:
-
Smoking (if you smoke you’re more likely to develop diverticulitis than someone who doesn’t smoke).
-
Having a close relative who has diverticular disease, particularly if they developed it before the age of 50.
-
Physical inactivity (if you’re not very active, it also increases your risk of constipation, which itself is a risk factor for developing diverticulitis).
-
Being overweight or obese. Discover some simple tips for weight loss in our helpful guide.
-
Using non-steroidal anti-inflammatory drugs (NSAIDs), such as the painkiller ibuprofen - though the reason this increases your risk isn’t clear (iii).
Eating a Western diet, with its typically low levels of fibre, has also been associated with the development of diverticular disease and diverticulitis. The NHS acknowledges that, while it isn’t yet known why diverticula develop, they are associated with not eating enough fibre (i).
This may be because the less fibre you eat, the smaller your stools, which means your intestine has to work harder to push them along, causing straining. And over the years, this straining - which also happens with constipation - may lead to diverticula.
The NHS also acknowledges that, while it isn’t yet known why diverticula develop, they are associated with not eating enough fibre.
Diet and diverticular disease/diverticulitis
If not eating enough fibre can promote the development of diverticular disease and diverticulitis, it’s easy to see why eating a high-fibre diet is often recommended to help prevent them – it may also improve your symptoms if you’ve already developed one of the conditions. There is also some evidence that eating lots of fibre and less fat and red meat may help prevent diverticular disease (iv).
Eating more fibre can help to prevent constipation, which is thought to be a factor in the development of diverticula. The latest advice from the government is that everyone should be eating 30g of fibre a day – though according to the NHS the average person eats just 18g a day (v). To eat 30g fibre you need to have the equivalent of five portions of fruit and vegetables, two whole-wheat cereal biscuits, two thick slices of wholemeal bread and a large baked potato with the skin on.
Other examples of high-fibre foods include the following:
-
High-fibre breakfast cereals (including porridge)
-
Baked beans, lentils and pulses
-
Brown rice and wholemeal pasta
-
Dried fruits
-
Wholemeal crackers and crispbreads
-
Nuts
At the same time, try to avoid low-fibre alternatives, such as white or brown bread, white pasta, sugary breakfast cereals, white rice, boiled potatoes without their skins and baked foods made with white flour, such as cream crackers, cakes and biscuits.
Good fibre sources
Fruit is an ideal source of fibre: just one medium pear (unpeeled) contains almost 4g of fibre, while an avocado contains almost 5g. Dried fruits are also high in fibre (three whole dried apricots contain 5g and three whole prunes contain 4.6g - but don’t overdo it, as dried fruits are also high in sugar. Beans, meanwhile, are full of fibre, with half a can of baked beans providing more than 7g.
A medium-sized bowl of All-Bran, however, is one of the best sources, providing almost 10g of fibre. Aim to increase your fibre intake gradually over a few weeks, as loading your digestive system with lots of fibre at the same time could lead to side effects such as bloating and wind.
But if you find it difficult to get the right amount of fibre in your diet, there are fibre supplements you could try (your GP can recommend one that would be suitable).
As well as eating plenty of fibre, experts also recommend drinking plenty of fluids, as this can also help prevent constipation (drink at least six glasses each day).
Staying as active as possible may also help, as exercise is thought to encourage regular bowel movements. Aim for at least 150 minutes of moderate-intensity activity each week, spread throughout the week (half an hour’s exercise five times a week, for example).
Treatments for diverticular disease and diverticulitis
If you don’t have any symptoms but have been diagnosed with diverticula - after having a colonoscopy, for instance - no treatment is necessary (though you will always have diverticula unless they are surgically removed).
Treatments for diverticular disease include taking paracetamol to relieve pain (other painkillers such as aspirin and ibuprofen are not recommended). Over-the-counter remedies such as bulk-forming laxatives may also provide relief if you’re constipated.
Your doctor may advise you to eat a high-fibre diet to manage your symptoms too, though it make take time before you’ll notice any improvements.
Cases of mild diverticulitis can also be easily treated with the following:
-
Paracetamol for pain relief
-
Antibiotics to treat infection
-
A liquid-only diet or low-fibre diet until your symptoms improve
Experts recommend a bland low-fibre diet for mild diverticulitis because it may help prevent further bowel irritation when you’re having a flare-up. However this should only be a short-term measure, and as your symptoms get better you should gradually re-introduce high-fibre foods into your diet.
Natural remedies for Diverticulitis
FOS
Those who struggle to eat the right amount of fibre may benefit from taking a natural fibre supplement, such as inulin and fructo-oligosaccarides (FOS). FOS - found in foods such as asparagus, Jerusalem artichoke, leeks, onions and soya beans - is closely related to inulin, also a soluble fibre, which is extracted from plants including chicory root. Both may help by keeping your bowels regular and by speeding up the movement of waste matter through your digestive system.
However, it’s advisable to stop taking any form of fibre supplements if you’re having an active flare-up of diverticulitis, as during this time your bowel needs to rest.
Glutamine
Another natural supplement that may be useful is glutamine (or L-glutamine), an amino acid derived from glutamic acid. Glutamine is believed to help keep your digestive system healthy - as well as playing a role in the effectiveness of your immune system and other bodily functions - by feeding the cells that line the intestines (enterocytes). As well as keeping the gut lining healthy, many natural health practitioners believe it may reduce inflammation, which in turn may provide relief from diverticulitis symptoms.
Omega-3s
Meanwhile omega-3 fatty acids - including eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) derived from fish oils - may also help reduce inflammation, and are thought to be useful in the management of inflammatory conditions (vi). High-strength fish oil supplements may be particularly useful for those who cannot or do not want to eat oily fish such as salmon, pilchards, sardines, herring and mackerel on a regular basis. Meanwhile if you’re a vegetarian or vegan you can still benefit from an omega-3 supplement, thanks to the availability of products that contain the natural triglyceride (TG) form of omega-3, which is sourced from plant organisms called microalgae rather than fish oils.
Peppermint
Finally peppermint oil capsules may provide relief relieving spasms, as it’s thought to help relax the smooth muscle of the intestinal tract (vii). For instance, studies suggest adding peppermint oil to a barium enema makes digestive spasms that such an enema commonly causes less severe (viii). Another study claims peppermint oil may reduce stomach spasms caused by a surgical procedure called an upper endoscopy (ix).
Managing diverticular disease may be difficult, but this article should help get you on the right track. If you’d like more information on a range of common health conditions, our health library is a good place to start.
References:
-
Available online: https://www.nhs.uk/conditions/diverticular-disease-and-diverticulitis/
-
Available online: https://patient.info/doctor/diverticular-disease
-
Strate LL et al., Use of Aspirin or Nonsteroidal Anti-inflammatory Drugs Increases Risk for Diverticulitis and Diverticular Bleeding. Gastroenterology. 2011 May;140(5):1427-1433.Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3081980/
-
Aldoori. W, Ryan-Harshman. M. Preventing diverticular disease. Review of recent evidence on high-fibre diets. Can Fam Physician. Circulation. 2002;48:1632-1637.
-
Available online: https://www.nhs.uk/live-well/eat-well/how-to-get-more-fibre-into-your-diet/
-
Simopoulos. AP. Omega-3 fatty acids in inflammation and autoimmune disease. J AM Coll Nutr. 2002 Dec;21(6):495-505.
-
Chumpitazi. BP, Keams. G, Shulman. RG. The physiologic effects and safety of Peppermint Oil and its efficacy in irritable bowel syndrome and other functional disorders. Aliment Pharmacol Ther. 2018 Mar;47(6)110:738-752.Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5814329/
-
Sparks. MJ, O'Sullivan. P, Herrington. AA, et al. Does peppermint oil relieve spasm during barium enema? Br J Radiol. 1995;68:841-843.
-
Asao. T, Kuwano. H, Ide. M, et al. Spasmolytic effect of peppermint oil in barium during double-contrast barium enema compared with Buscopan. Clin Radiol. 2003;58:301-305.
-
Hiki. N, Kurosaka. H, Tatsutomi. Y, et al. Peppermint oil reduces gastric spasm during upper endoscopy: a randomized, double-blind, double-dummy controlled trial. Gastrointest Endosc. 2003 ;57:475-482.
Related Posts
Disclaimer: The information presented by Nature's Best is for informational purposes only. It is based on scientific studies (human, animal, or in vitro), clinical experience, or traditional usage as cited in each article. The results reported may not necessarily occur in all individuals. Self-treatment is not recommended for life-threatening conditions that require medical treatment under a doctor's care. For many of the conditions discussed, treatment with prescription or over the counter medication is also available. Consult your doctor, practitioner, and/or pharmacist for any health problem and before using any supplements or before making any changes in prescribed medications.

Christine
Christine Morgan has been a freelance health and wellbeing journalist for almost 20 years, having written for numerous publications including the Daily Mirror, S Magazine, Top Sante, Healthy, Woman & Home, Zest, Allergy, Healthy Times and Pregnancy & Birth; she has also edited several titles such as Women’ Health, Shine’s Real Health & Beauty and All About Health.
View More